The Adaptation of Pediatric Exercise Testing Programs to the COVID-19 Pandemic
By Adam Powell
In mid-December 2019, a novel strain of coronavirus (COVID-19) was discovered and quickly spread throughout the world. As a result, there were several regional and national initiatives in the United States aimed to lessen both loss of life and the strain on the hospital systems caring for these patients. In the hospital, much of the focus was placed on the strategies to care for the hospitalized patients with COVID-19. As a by-product of these changes, alterations in the outpatient care of non-ill patients profoundly affected the routine surveillance and treatment of patients with cardiac conditions.
Cardiopulmonary exercise testing (CPET) is a valuable tool to understand how the heart and lungs respond to the stress of exercise and is often used in the care of both children and adult patients with known or suspected heart disease. The exercise laboratory is in a unique position compared to other areas of the hospital in that the possible aerosolization of particles that occurs during exercise may infect patients, family, and staff. Even now the risk of spreading COVID-19 during an exercise test remains unclear. Additionally, while early in the pandemic there was near consensus on certain clinical scenarios, such as the need to delay elective surgeries, there was minimal guidance issued for the administration of exercise testing. This resulted in large variability in practice between pediatric exercise laboratories.
In writing “The Adaptation of Pediatric Exercise Testing Programs to the Coronavirus/COVID-19 Pandemic”, we sought to better understand the practice patterns of pediatric exercise testing laboratories in the beginning of the COVID-19 pandemic. To do this, questionnaires were sent to pediatric CPET laboratories throughout the United States and Canada. There were responses from 41% (35/85) of programs across a wide geographic area. The responses showed a lack of unified response on how to minimize exposure to patients and staff. For example, 68% of exercise laboratories stopped all testing by May 2020 despite only 9% of programs having an employee that tested positive or was exposed to COVID-19. Of the programs that closed, 23% had no plans to reopen as of May 2020. In polling the 77% of programs that continued or planned to restart exercise testing:
Personal protective requirements included 96% requiring gloves, 88% surgical masks, 69% face shields, 62% gowns, and 54% N-95 masks.
47% of these programs either ceased or modified metabolic measurements during CPET.
Of the 26 programs that performed pulmonary function testing in conjunction with CPET, 62% either stopped or modified this testing.
A major reason for the heterogeneity in responses likely arises from the lack of consensus whether exercise testing is an aerosol producing procedure. With no national guidance, some hospitals have deemed CPET as high-risk for aerosolization with resultant N-95 requirements and alterations of protocols, while other hospitals who feel the aerosol risk is low only require basic personal protective equipment. Likely because of this confusion, almost 60% of programs voluntarily disclosed in the comment section on the questionnaire that they would like additional guidance on how to perform exercise testing safely.
While this study was performed very early in the pandemic, the lack of a unified exercise testing response remains today. There continues to be no true consensus on the infectious risk of exercise testing, although some groups are seeking to remedy this. Additionally, while the tools to care for COVID-19 patients have increased with improved access to pre-procedure COVID-19 testing and the creation of an effective immunization, the lack of a clear consensus on how to use these tools has resulted in even more practice variability. This needs to be remedied to ultimately determine the safest and most effective way to care for cardiac patients during this prolonged pandemic. Additional research is needed on the aerosolization of particles during exercise testing, and in the absence of this evidence expert consensus statements should be created to assist the exercise laboratory in caring for patients during the COVID-19 pandemic.
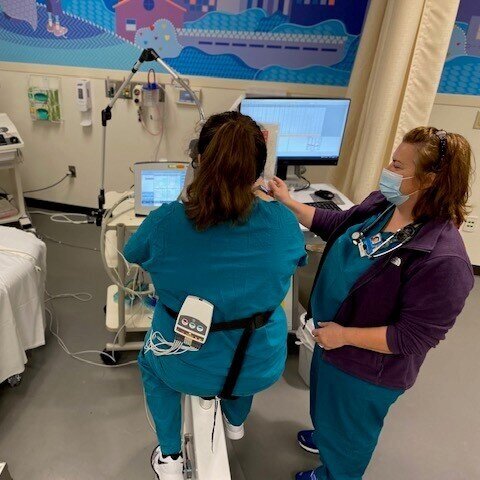
Cardiopulmonary exercise testing being performed on a patient during the COVID-19 pandemic. Patient previously tested negative for COVID-19 prior to this test. Photo by Sandra Knecht.
Article details
The Adaptation of Pediatric Exercise Testing Programs to the Coronavirus/COVID-19 Pandemic
Adam W. Powell, Wayne A. Mays, Tracy Curran, Sandra K. Knecht, Jonathan Rhodes,
First Published September 21, 2020
DOI: 10.1177/2150135120954816
World Journal for Pediatric and Congenital Heart Surgery
About the Author